For every surgery, the surgeon is of paramount importance. In LASIK and SafeSight TransPRK a capable surgeon will keep surgical complications in check. Furthermore, reduced time taken during surgery done by a capable surgeon will result in an accurate results. As such, you may want to make sure the surgeon is well capable in laser refractive procedures and is board certified. You may also want to check if he has a good reputation in the community, and if he is committed to his patients before, during and after the surgery.
Frequently Asked Questions
Most Frequently Asked Questions:
No, the procedure is done completely under local anesthesia via eye drops. The eye drops are instilled just before the surgery and will numb the eyes so that there is no pain felt throughout the procedure.
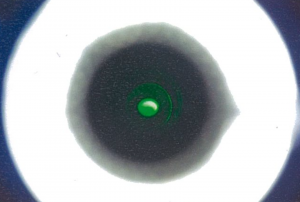
During the surgery, you will be tasked with one simple but important job – to focus your gaze on the blinking green light (this is a guiding light to help you look in the direction of the laser) while the laser is active. Try to relax, do not squint, and do your best to keep your eye from moving around. This helps the procedure to go quickly and smoothly and ensures a great result.
Green Fixation Light
If you’re a contact lens wearer, you must stop wearing them for 3 days for soft contact lens and 10 days for hard contact lens/ Ortho-K lens) prior to the appointment.
If you’re a contact lens wearer, you must stop wearing them for 3 days for soft contact lens and 10 days for hard contact lens/ Ortho-K lens) prior to the surgery.
The results for your eye evaluation are valid for 6 months. This is because your eye condition might be different after 6 months, requiring you to undergo another comprehensive eye evaluation to ensure the accuracy of your treatment.
You should rest at home and observe good hygiene. Do not touch your eyes and eyelids with dirty hands or apply the prescribed eyedrops without first washing your hands clean. Avoid crowded and dirty places and take care to ensure that dirty water from washing your face or hair do not get into your eyes. You should also refrain from rubbing your eyes for the first five days post surgery. At this first sign of severe pain or redness of the eyes or abnormal eye discharges, you should contact your eye doctor for an immediate eye review to avoid an eye infection.
No, please do not drive to the clinic as your vision may be blurry after surgery and your eyes may feel some discomfort. If possible, arrange for someone to accompany you to the clinic on your surgery day, or book a Grab ride. If you need help requesting a Grab ride, our staff will be happy to assist.
There is no minimum power i.e. people with 100 degrees of myopia can still go for refractive surgery. The maximum power for safe myopia correction is usually limited to 1,300 degrees. For astigmatism, we usually do not treat patients with more than 400 degrees of astigmatism. For hyperopia of more than 300 degrees or for those suffering from more than 1,300 degrees of myopia, lens implant or ICL surgery is the suitable option.
Many patients will find that they are able to see clearly without the need to wear glasses or contact lenses after laser vision correction. But there is no absolute guarantee that you do not need to wear glasses after surgery. For those patients with high powers, sometimes residual power remains that may require glasses to be worn to achieve 6/6 or perfect vision. When glasses need to be worn after surgery, they will be of significantly reduced power and dependence.
Enhancement surgery may be recommended for some patients who have significant amounts of residual eye power six months or more after the initial procedure. However, this depends on whether there is enough cornea tissue thickness to allow safe enhancement. For ReLEx SMILE patients, enhancement is possible only through a different technique i.e. Advanced Surface Ablation methods such as SafeSight TransPRK. For LASIK patients who need enhancements, if the residual cornea thickness beneath the flap is too thin, Advanced Surface Ablation methods such as SafeSight TransPRK can be done on the flap surface.
Most people have the misconception that the laser itself is what could cause the blindness (from watching horror movies etc.) But in reality, eye infection after the surgery is the real cause of any form of complications leading to visual impairment. That being said, it is very rare and if infection does occur, it is typically minor.
When laser vision correction started, the industry standard was to do one eye at a time. However with advances in technology and technique, it is acceptable and safe to go for bilateral laser vision correction as the risk of serious simultaneous bilateral complications is low. Today, Many patients (over 98%) will opt to do the surgery on both eyes at the same time for convenience in terms of taking medical leave and having to go through the discomfort of the recovery process twice. Furthermore, if patients opt to do one eye at a time, they will feel the discomfort and disruption of having imbalance vision during the interim period between the first and the second eye.
The procedure is contra-indicated in pregnancy. Women who are breastfeeding should not go for the procedure unless the baby is over eighteen months of age where the risk of eye drops medications affecting the child is low. But if you want to be completely safe, go for the surgery only after you have stopped breastfeeding your child.
Yes, soft contact lenses, including cosmetic lenses can still be worn but only after 3 months. Hard lenses cannot be worn as they tend to slip due to the altered cornea curvatures.
Yes and no. Your treatment is permanent, but as with every part of your body, your eyes will continue to age and your vision will be affected as you get older. Laser vision correction cannot prevent cataracts and presbyopia, but most patients enjoy many years of focused vision without glasses and contacts.
No, as laser vision correction surgery and cataract surgery take place at a different parts of the eye. Your eye surgeon will need to factor in the new cornea curvature when making the calculation and selection of the intra-ocular lens implant for the cataract surgery.
Medisave cannot be used to claim for laser vision correction as the procedure falls under the category of an “elective” procedure.
Yes. Since 2001, we have provided minimally invasive laser vision correction surgery that has been proven to create clear vision, safely for our patients. As with any surgical treatment, there are possible risks and side effects. After a thorough eye exam and consultation, we will discuss your options with you and help you make the right decision for your vision.
LASIK is also known as the flap-and-zap method. During LASIK, a cut is made across the cornea such that a flap is created. The flap is then lifted, and laser correction will be applied to the underlying cornea tissue. After which, the flap is closed back without any form of stitches.
On the other hand, in SafeSight TransPRK, there’s no cut is made to the cornea. The uppermost surface layer of cells – also known as the epithelium layer – is removed using excimer laser. The same excimer laser is then applied to the underlying cornea. As the epithelium cells have regenerative properties, these cells will grow back on its own in 3-5 days. In this way, corneal tissue loss and nerve damage can be effectively preserved.
You will need to go through an in-depth pre-TransPRK evaluation, where the optometrists and eye doctor will check your eyes thoroughly. In general, these are some of the factors that determines your suitability: (1) cornea shape (2) cornea thickness (3) any existing eye conditions such as glaucoma, cataracts, etc.
Corneal thickness must be at least 485 microns thick.
If you have myopia, your prescription must not be more than -10 diopters (1,000 degrees).
For hyperopia, not more than -4 diopters (400 degrees).
For astigmatism, not more than -5 dioptres (500 degrees).
For hyperopia of more than 300 degrees or for those suffering from more than 1,300 degrees of myopia, lens implant or ICL surgery is the suitable option.
You may want to opt for SafeSight TransPRK over LASIK if:
- You do not want to cut a cornea flap.
- You do not want to suffer from flap related complications such as flap infection, inflammation and flap dislodgement or flap wrinkles.
- You do not want to worry about suffering from dry eyes after LASIK as the cornea nerves are not cut.
- You have an active lifestyle and participate in contact and rugged sports such soccer, rugby, water skiing, competitive basketball or martial arts where the risk of traumatic cornea flap damage is higher.
- You want to preserve precious cornea tissue effectively for possible upgrade surgeries in future as your eyes age naturally. (such as future “lao hua” or presbyopia surgery)
Length of surgery: about 5 minutes per eye
- Put on your surgical gown and other PPE
- Lie flat and get comfortable on the operating bed.
- A clamp is then used to keep your eyelids open
- Numbing eye drops are added so that your eye does not feel anything
- Your eye is lined up in the optimal position for the laser
- Stare straight at the dim green light

Schwind Fixation Light
- The laser starts to ablate the surface cells
- The laser then starts to reshape the cornea
- Your vision has been corrected!
- A bandage contact lens is placed over the eye to allow the surface cells to safely heal (to be removed after 5 days by the doctor)
SafeSight TransPRK only takes approximately 5 to 6 minutes per eye, while standard LASIK takes 10 minutes to 15 minutes per eye, about double the time – mostly due to the additional stage of cutting of the cornea flap.
TransPRK surgery is painless! This is because numbing eye drops are applied to your eyes before the surgery. There are no injections involved.
TransPRK surgery is quick – it only takes 3 – 5 minutes for your vision to be corrected. Some patients report that they feel a slight pressure in their eyes, but no pain.
Modern LASIK and SafeSight TransPRK is safe and problem-free in the vast majority of cases. However, there is no such thing as risk free surgery. The surgery will have the risk of complications such as infections, inflammation, acute dry eye, under/over correction, glare, halos and starbursts. Such conditions, however, do not occur often. Nevertheless, to ensure a smooth recovery, patients should also do their parts by following the doctor’s post-surgery instructions diligently.
Because there is a cut made across the cornea, LASIK has the additional risk of flap complications. These include: flap infection, flap inflammation, risk of flap dislodgement caused by rubbing or a finger poke or sports injury. Another complication resulting from a cut flap is acute and chronic dry eye because of the thousands of tiny cornea nerve endings are being severed in the process of cutting the cornea flap.
Patients often return to most of their daily activities, including going back to work, 1 week after their TransPRK treatment.
Post-TransPRK, you will be allowed to resume these activities after a specific period of time:
Long sessions of reading books, screens and watching TV: 12 hours
Driving: 1 week
Applying eye makeup : 1 week
Eyes having to avoid water while showering: 1 week
Swimming and other water-related activities: 2 weeks
Light sports: 1 week
Contact sports: 2 weeks
You will be given up to 5 days of MC, including the day of the surgery itself. Many patients report that they see and feel well and are tempted to go back to work early. However, it is advisable not to go back to work the first three days after the operation so as to reduce the risk of infection and to put in the prescribed eye drops at the prescribed intervals for fast and safe recovery.
Yes. The common strategy for those who have presbyopia is to aim for close to perfect vision in the dominant eye (usually the right eye) and deliberately aim for some under-correction in the other eye. This strategy is sometimes called “monovision correction”.
This is one of the most common questions we hear, and many patients want to know which treatment is “better.” The fact is that both TransPRK and SMILE are proven and consistent, so most patients will be very happy with either option.
Generally speaking, TransPRK has the benefit of having no surgical equipment touch the eye, resulting in a shorter surgery. TransPRK is also able to treat a wider range of conditions. On the other hand, SMILE has a shorter downtime after surgery and little to no discomfort while recovering. You will be able to go back to work in just 2 – 3 days. Based on your eye structure and lifestyle goals, your surgeon can recommend the right treatment for you!
For more information, read this article we made comparing the two procedures!
You will need to go through an in-depth pre-SMILE evaluation, where the optometrists and eye doctor will check your eyes thoroughly. In general, these are some of the factors that determines your suitability: (1) cornea shape (2) cornea thickness (3) any existing eye conditions such as glaucoma, cataracts, etc.
Corneal thickness must be at least 550 microns thick, meaning that thinner corneas might not be eligible.
If you have myopia, your prescription should be between -2.5 to -8 diopters (250 – 800 degrees).
Hyperopia is not treatable by ReLEx SMILE.
For astigmatism, it should not more than -2.5 diopters (250 degrees).
SMILE and TransPRK use different laser technologies to recreate the clarity of your vision, the costs of the two options are different. These costs account for the skill and experience of your surgeon, the costs and fees of acquiring and using the laser technologies, and the costs of the support staff and surgical follow-up.
Yes. The FDA (Food and Drug Administration) approved SMILE for the United States in September 2016 after rigorous trials and testing showed it to be a consistent, effective way to improve vision and reduce dependence on glasses and contacts.
ReLEx SMILE is not a different version of LASIK. They are in fact two different types of laser vision correction methods. Since it was introduced to the world in the 1990s, LASIK has gained worldwide popularity, which is the reason why most people refer to any form of laser vision correction as “LASIK”.
Length of surgery: about 10 minutes per eye
- Put on your surgical gown and other PPE
- Lie flat and get comfortable on the operating bed.
- A clamp is then used to keep your eyelids open
- Numbing eye drops are added so that your eye does not feel anything
- Your eye is lined up with the suction cup
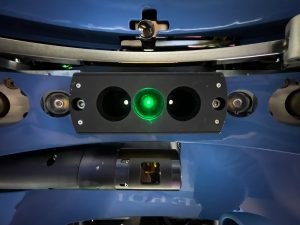
- Stare straight at the dim green light

ZEISS Fixation Light
- The laser creates a lenticule (small lens shaped piece of corneal tissue)
- The laser then makes a small micro-incision of 3.5 mm
- The lenticule is removed through this small incision, changing the shape of the cornea
- Your vision has been corrected!
SMILE surgery will take around 10 – 15 minutes per eye.
SMILE is a gentle vision correction solution. Patients consistently tell us it was very comfortable. Some patients do say they feel a tiny amount of pressure around their eye for a few seconds during the treatment, but are quick to clarify that it didn’t hurt at all!
Patients often return to most of their daily activities, including going back to work, 2 days after their SMILE treatment.
Post-ReLEx SMILE you will be allowed to resume these activities after a specific period of time:
Long sessions of reading books, screens and watching TV: 12 hours
Driving: 48 hours
Applying eye makeup : 48 hours
Eyes having to avoid water while showering: 48 hours
Swimming and other water-related activities: 2 weeks
Light sports: 5 days
Contact sports: 2 weeks
You will be given up to 3 days of MC, including the day of the surgery itself. Many patients report that they see and feel well and are tempted to go back to work early. However, it is advisable not to go back to work the first three days after the operation so as to reduce the risk of infection and to put in the prescribed eye drops at the prescribed intervals for fast and safe recovery.
SMILE is not able to treat presbyopia.
Book Your Eye Evaluation
If you would like to book a suitability evaluation with us to determine if you are eligible for laser vision correction surgery,
📞 Call us at 6733 3316
📱 WhatsApp us at 8383 7989
✉️ Email us at doctor@clearvision.com.sg
🤳 Message us on Facebook
🤳 Message us on Instagram
The evaluation costs $55 and will take around 1 – 2 hours.
It will include a series of eye tests as well as a personal consultation with your lasik surgeon.
Suitability Evaluation Guide
Our suitability evaluations typically take place during these times, subject to availability –
| Mondays | 2:30 PM – 3:30 PM |
| Tuesdays | 9:00 AM 2:30 PM – 5:15 PM |
| Wednesdays | 9:00 AM |
| Thursdays | 2:30 PM – 3:30 PM |
| Fridays | 9:00 AM – 11:00 AM 2:30 PM – 5:15 PM |
Just let us know which days and times work for you and we’ll do our best to accommodate.